I was 13 when I went on my first diet.
I had been struggling with my weight for about six years, and my obsession with how I looked was starting to dominate my life.
I only had two to three shirts that I felt comfortable in. The only thing that mattered was that they didn’t make me “feel fat.” Even those chosen shirts were always under my West 49 sweater, for extra coverage.
The cherry on top of this presentation was my slouched shoulders—a defense mechanism to protect against exposing my “man boobs,” the body part that had dynastic reign for being my biggest insecurity.
The way I viewed my body governed my self-worth.
I felt that my body held me back from enjoying countless moments of my life, and by the ripe age of 13, I decided I was sick of it.
I figured the only way I could change this purgatory was by changing my body.
I started exercising three to four times a day. For my first two meals a day, I drank a sludge of water mixed with “weight loss smoothie powder” (really just a glorified protein shake). Whenever I “cheated,” I punished myself the next day by eating even less or exercising even more.
In about 5 months, I lost 60 lbs. One third of my body weight to be exact.
This was how I spent the summer transitioning from elementary school to high school. Counting calories over making memories.
To no surprise, this was met with endless praise. And it felt good. Scratch that, it felt incredible.
I had experienced both sides now: One where I felt valueless because I was in a fatter body, and one where I felt accepted and prized because I was in a thinner body.
In another version of this story, I might’ve learned something from my newly widened perspective: I might’ve gained empathy, seeing the unfair stigma projected at people in larger bodies. I might’ve gained bravery, advocating for more body acceptance, regardless of someone’s size.
But instead, I participated in the problem.
I built up the identity of being a “former fat person” who is proof that “anybody can lose weight.”
However, as this script typically goes, over the next few years, I gained a lot of the weight back.
This sent me into a depression. I felt like I had lost my value; like I had won the lottery and blew through my fortune.
That was the pattern I repeated for almost 15 years.
Until I stumbled on something called “body neutrality.”
For me, adopting a more body-neutral approach created a paradigm shift—it offered a way to uncouple my appearance with my happiness. It also caused me to ask some deep questions about my body, and the kind of life I wanted.
Questions like:
“Do I want my self worth to be defined by my external appearance?”
“Do I want to continue this cycle—and potentially pass it on to any future kids I might have?”
“What would my life look like if I fought to value myself for who I am as opposed to what I look like?”
My answers weren’t immediately clear. But body neutrality created an opportunity to step off the hamster wheel of chasing aesthetic goals—and finally, truly reflect.
In this article, I’ll walk you through the process of adopting a more body neutral approach to your own self image and self-care.
You’ll learn:
- What body neutrality is
- How to think about your body and your health—in a way that isn’t dependent on appearance
- Five actionable, body neutral strategies you can apply today—if you want to stop letting your weight, size, or shape dictate your happiness
Let’s begin.
What is body neutrality?
Body neutrality is a mindset that encourages you to value how your body functions and feels over how it looks. This perspective helps you develop self-acceptance, while still working to care for yourself in ways that promote overall health.
In practice, this looks like:
✅ You exercise and eat nutritiously—not because it makes you look a certain way—but because it makes you feel good.
✅ You still have treats (because life is too short to be deprived of pizza!) but you don’t eat them to excess because they don’t make you feel the best, physically.
✅ You wear clothes and celebrate your appearance in ways that feel authentic, but how you “display” yourself isn’t the foundation of your self-worth.
✅ You don’t always love all aspects of your body, but you don’t let that stop you from enjoying your life; Improving your appearance doesn’t “earn” you the right to be happy.
✅ You might still care about how you look, but you broaden your self-concept so it also includes your values and your inherent worthiness as a human.
I value seeing friends and family. I value playing rec sports. I value new experiences.
When I’ve been heavier, I’ve neglected these things in favor of isolating myself.
“I’ll do them again when I lose weight” is something I’ve uttered to myself more times than I can count.
Body neutrality helped me realize I still deserved these things—no matter how I looked.
Everyone can benefit from body neutrality.
Body neutrality isn’t just for people in larger, or otherwise marginalized bodies.
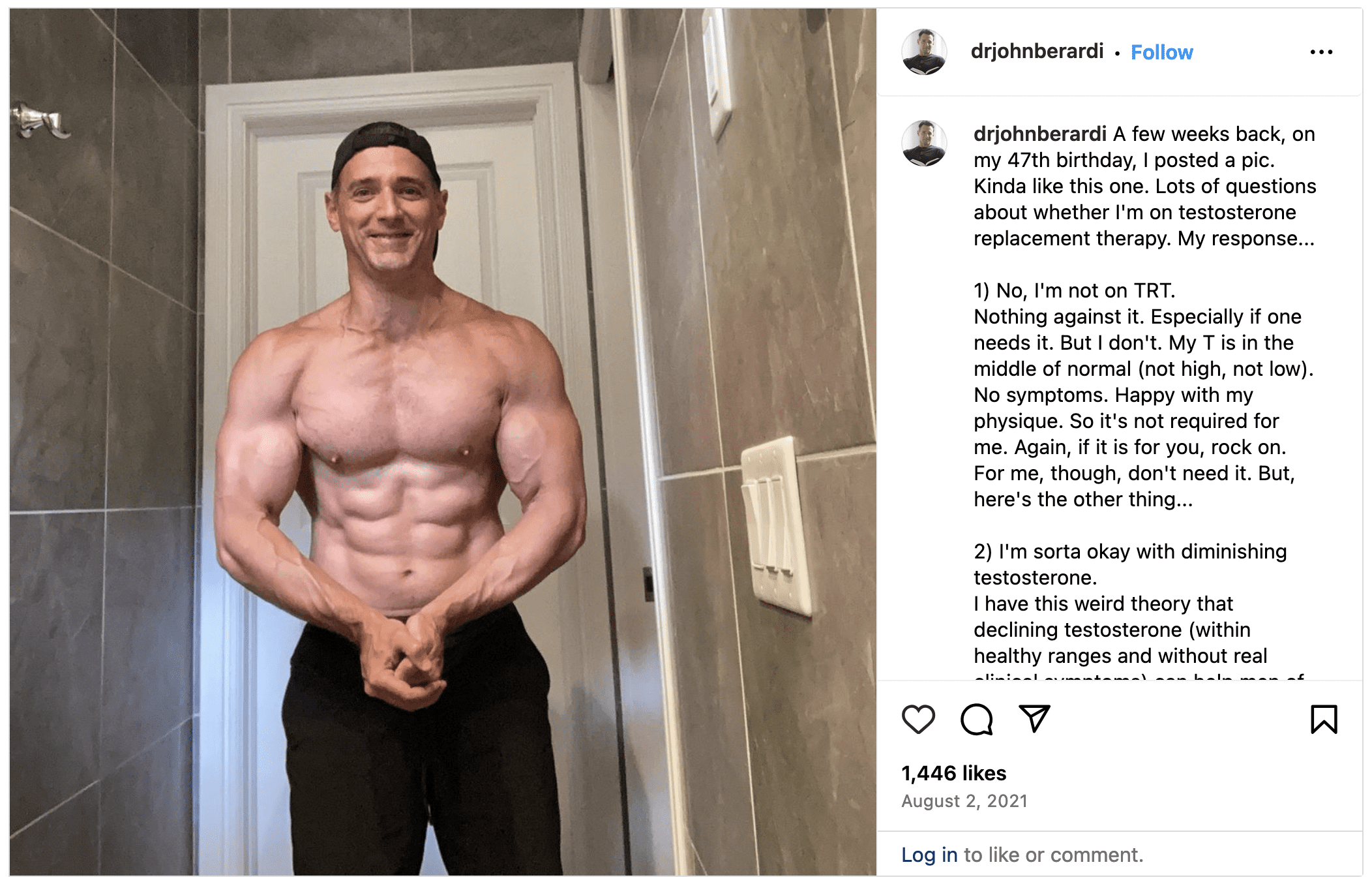
It’s also useful for people with “ideal bodies,” who’ve been the recipients of validation and privilege because of the way they look.
“I’ve worked with clients who are fairly satisfied with their appearance, but they still struggle with their body image because their self-worth relies on it,” says Shannon Beer, registered nutritionist and body image coach.
People with idealized bodies sometimes aren’t living the life they want either, because they have to exhaust their energy to maintain an image of “perfection.”
(If you want to know what kind of sacrifices it takes to meet those “ideal” standards, check out: The cost of getting lean: Is it really worth the trade-off?)
“The ‘meh’ is the magic.”
That’s a quote from Jessi Kneeland, body neutrality coach and author of Body Neutral: A Revolutionary Guide to Overcoming Body Image Issues, when they sat down with some PN coaches to talk about body-neutrality.
(Want to listen in on the whole conversation? Watch it here: PN Coaches discuss body neutrality and negative self-talk)
The goal with body neutrality isn’t to love your body and all of its parts all of the time. Nor is it to be so toxically positive that you ignore real—and sometimes negative—feelings about your body.
That just isn’t realistic for most people.
Instead, an underrated goal is to feel sort of… meh.
You’re not overly glorifying or criticizing your body; its appearance just doesn’t hold that much importance.
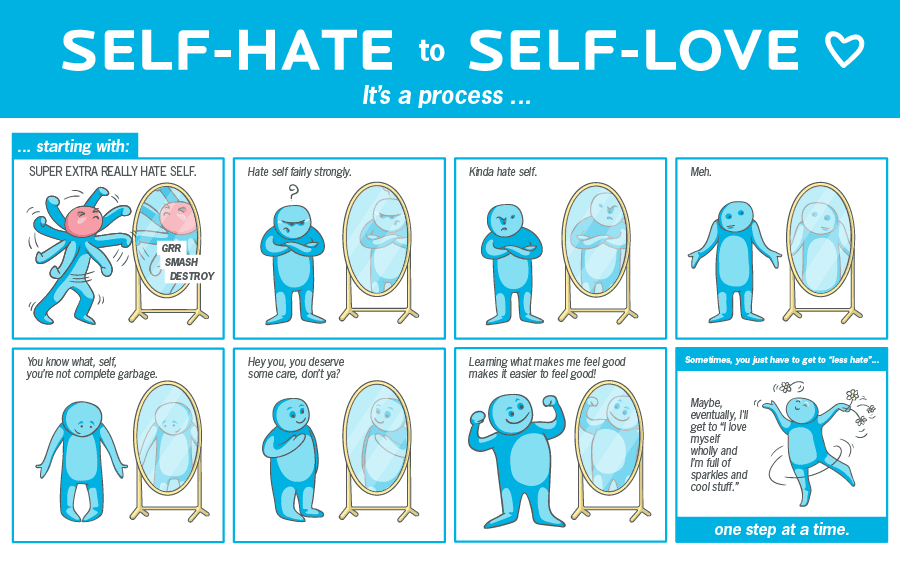
When you’re used to hating your body, getting to neutral (or ‘meh’) can actually be hugely freeing. From there, you may learn to appreciate yourself in a deeper, less appearance-centric way.
In practice, you may love certain parts about your body—but also feel ambivalent or mildly negative about other parts.
For example, you may see your stomach and feel ashamed because you don’t like what you see.
This feeling is uncomfortable, but it’s not “right” or “wrong.” You just don’t want that feeling to dictate your behavior. (Such as seeing your stomach and then saying, “Alright, I’m not going out tonight,” or, “Diet starts tomorrow!”)
To give you a personal example:
As a dude living in North America, I feel pretty ‘meh’ about being 5’9” tall.
Would I love to be 6’2”?
Sure.
But I’m not 6’2”—and I can’t change that. My height won’t ruin my day and I surely won’t be depriving myself from the things I enjoy most in this life because of it.
Body neutrality and aesthetic goals
Some people worry that if they adopt a more body neutral approach to their health and fitness, it means they have to relinquish any desire for physical change.
They also might worry that being more body neutral might make them lose certain aspects of their appearance that they like (such as muscular legs or a slim torso).
Here’s the thing: Body neutrality advocates for health.
Being body neutral doesn’t mean your body can’t change.
It just means your self-worth isn’t dependent on that change, and that your whole life isn’t consumed by the pursuit of a physique goal.
If you’ve been starving yourself and overexercising to the point of burnout, body neutral principles will encourage you to disengage from those extreme activities in the pursuit of a specific physique.
If you’ve been overeating and avoiding exercise because you can’t stand your body, body neutral principles will encourage you to tune into your genuine sense of care and love for yourself, and help you choose food and movement that support your body—regardless of its shape.
In this sense, body neutrality can have a balancing effect on health and fitness behaviors, and, according to Beer, is unlikely to take away from physical health, if applied correctly.
Plus…
There’s nothing inherently wrong with having an aesthetic goal.
Body neutrality rejects physical or aesthetic change only if it’s to the detriment of your overall mental, emotional, social, physical, and existential health.
5 things you can do today to be more body neutral
Congratulations: Just setting the intention to step away from an appearance-centric approach to health and fitness is a great start.
But, ultimately, it’s only action that creates deep, lasting change.
So, here are five tangible strategies you can work on immediately to develop a more body neutral approach.
Strategy #1: Do the things you love today.
Stop waiting to achieve the “ideal” body in order to be able to enjoy your life, and start doing more of what you love now.
Start with something easy that you tend to stop yourself from doing when you feel insecure about your appearance.
When I was in my worst spots, I stayed inside too much—even though I love being outside. It might sound silly but even reading outdoors in nice weather was helpful for me.
The point is: It can be that small.
Find one thing you’ve deprived yourself of in the past and do it—even if it’s a small dose, regardless of how you feel. Re-teach yourself that you don’t need a certain body shape or size to allow joy into your life.
(If you want more ideas on how to stop thinking you’re simply [insert thing you think you need] away from being happy, check out: “I’ll be happier when I lose weight” is a recipe for regret. Here’s the counterintuitive solution)
Strategy #2: Set body-neutral goals.
This is a gamechanger in my coaching experience. I’ve seen clients transform their relationship with exercise when they focus more on what they can do as opposed to how they look. “I feel so much better but I haven’t lost any weight,” is a sentence I’ve heard repeatedly.
When you’re overly appearance-centered or focused on weight, you risk missing other indicators of progress—like how good you feel.
If your fitness goals tend to be aesthetic-centric, try setting a goal that has nothing to do with how you look.
This can look like:
▶ Setting strength and performance goals in fitness (such as beating a deadlift PR, or a sprint time)
▶ Practicing slow, mindful eating at more meals (if you usually inhale your meals in seven minutes tops, see if you can make a meal last 20 minutes, chewing your food well and savoring each bite)
▶ Working to develop a new a skill in the gym (like your first pull-up, or a cool Olympic lift, like a clean and jerk)
None of these depend on your appearance; They’re all focused on what you can do. (And chances are, you’ll feel more empowered than ever when you start achieving them.)
Strategy #3: Curate your environment.
Take control of the parts of your environment that feed the body-image obsessed wolf. Starve that beast wherever you can.
Here are some ideas:
▶ Unfollow social media accounts that prey on insecurity or promote unrealistic ideals. Follow more that are body-neutral, or inspire other aspects of your personality (like comedy, or crafting).
▶ See what it’s like to reduce your exposure to your own appearance. This can look like having fewer mirrors (or covering some up for a period of time), or turning off the self-view on Zoom.
▶ Consider ditching the scale. Most people struggle to stay “neutral” about whatever number that shows up.
▶ Set boundaries around body talk. Some environments are rife with commentary about body hang ups or goals. If someone begins talking about their new weight loss diet or “disgusting gut,” try changing the topic, or just exit the conversation. Eventually, people will realize you’re not the right audience.
Strategy #4: Find your people.
Body neutrality won’t be the most common approach you’ll run into in the fitness world.
But, intentionally seeking out and surrounding yourself with more body neutral folks can keep you from constantly getting sucked back into an appearance-centric mindset.
There are body neutral, body positive, or HAES (health at every size) community groups all over social media and the internet, and this can be parlayed into finding local groups near you too.
Seeking out these spaces will only provide more support—and positive momentum—as you pursue a more body neutral approach.
Strategy #5: Strive for improvement, not perfection.
You don’t need to be a body-neutral icon or master. The expectation is not that you 100 percent divest from focusing on your appearance.
Body neutrality exists on a continuum.
Assess where you are right now in terms of how appearance-centric you are when it comes to health and fitness. If all your eggs are in the “aesthetics basket,” then even taking one metaphorical egg out (and say, putting it in the “gardening” basket) is progress.
Use the list of suggestions above to set some small goals, and just begin where you can.
You might always care about your appearance (maybe even more than average), but if it’s progress from where you started, you’re winning.
What life on “the other side” looks like
Even after sharing all of this, I won’t sit here and lie to you by saying I’m pure-bred body-neutral, all the time.
But I like to think I’ve grown a lot since my days of hiding out inside during “fat days.”
I’m better at doing the things I love, even when I don’t feel confident in my body.
I’m better at wearing comfortable clothing when I don’t feel good about my body— instead of cramming myself into something that’s too tight and suffering all day.
And, I’ve expanded the way I see fitness for myself and my clients, focusing more on feel and function, rather than achieving a certain look.
For me, this is progress.
Yours might look different.
Be kind to yourself, and acknowledge that you might be working through decades of programming. Body neutrality sure isn’t a quick fix, but the lasting freedom, joy, and genuine sense of self-worth it offers is worth it.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)